INTRODUCTION
VR holds great importance in revolutionizing patient care
In a world where virtual reality (VR) has become synonymous with groundbreaking advancements in gaming and entertainment, its immersive experiences capture imaginations and set new standards for engagement. Players don headsets and step into fantastical realms, experiencing adventures that blur the line between reality and fiction. Yet, beyond the flashing lights and epic quests, VR quietly and profoundly transforms another arena: patient care.
Imagine a cancer patient, once dreading the hours of chemotherapy, now transported to a serene beach where the rhythmic sound of waves brings calm and comfort. Picture a stroke survivor who, instead of the tedious repetition of traditional rehabilitation exercises, finds themselves immersed in a vibrant virtual environment where recovery becomes an exciting journey. Visualize a young child with severe burns, their pain alleviated not by narcotics but by a captivating VR game that transports them to a world where pain no longer exists.
This is the revolutionary power of VR in healthcare. It reshapes how we approach medical treatment, offering innovative solutions that enhance patient engagement outcomes. Surgeons now use VR to simulate complex procedures, perfecting their techniques in a risk-free virtual setting before stepping into the operating room. Mental health professionals are leveraging VR to create controlled environments for exposure therapy, helping patients confront and overcome anxiety, PTSD, and phobias in a safe and supportive space.
Moreover, VR is proving to be a game-changer in pain management. By immersing patients in engaging and distracting virtual worlds, VR reduces pain perception and minimizes the need for pharmaceutical interventions. This is particularly beneficial for chronic pain sufferers and those recovering from surgery or injury, as it provides a non-invasive and effective alternative to traditional pain relief methods.
The potential of VR to revolutionize patient care is immense, but it comes with its own set of challenges. Issues such as cost, accessibility, and the need for specialized training for healthcare providers must be addressed to ensure that VR's benefits reach all patients. However, as technology evolves and becomes more integrated into healthcare systems, the dream of a fully immersive, patient-centered approach to medical care is becoming a reality.
As we venture further into the 21st century, the convergence of VR and healthcare is paving the way for a new era of medicine. By offering innovative, immersive, and personalized solutions, VR is not just enhancing patient care; it is revolutionizing it. This blog delves into the multiple ways VR transforms healthcare, from surgical training and pain management to mental health and rehabilitation, highlighting this cutting-edge technology's profound impact and promising future in patient care.
WHAT IS VR?
VR takes you to another world with a promise of better treatment
Virtual Reality (VR) in healthcare refers to using immersive, computer-generated environments to enhance various medical applications. This advanced technology enables users to experience and interact with three-dimensional simulations, creating realistic scenarios tailored for specific medical purposes. In healthcare, VR is harnessed for various applications, including surgical training, patient treatment, rehabilitation, pain management, and mental health therapy. By creating a virtual environment that can be manipulated and controlled, VR provides a unique platform for healthcare providers and patients to explore innovative treatment and training methods.
The journey of VR from a nascent technology to a cornerstone of modern healthcare is a testament to human ingenuity and the relentless pursuit of better patient outcomes. The origins of VR can be traced back to the mid-20th century, with the development of early flight simulators and rudimentary immersive experiences. However, it wasn't until the 1960s and 1970s that VR began to take shape, thanks to pioneers like Ivan Sutherland, who created the first head-mounted display system, and Morton Heilig, whose Sensorama machine offered a multi-sensory experience.
The 1990s marked a significant leap forward, as technological advancements and increased computing power made VR more accessible and practical. During this period, the potential of VR in healthcare began to be realized. Early adopters explored its use in surgical simulations, allowing surgeons to practice procedures in a controlled, risk-free environment. These initial forays laid the groundwork for the sophisticated applications we see today.
The turn of the 21st century brought about rapid advancements in VR technology, driven by improved graphics, processing power, and user interfaces. High-resolution displays, precise motion tracking, and more affordable VR systems catalyzed its adoption across various sectors, including healthcare. Researchers and medical professionals began to explore VR's potential in areas such as pain management, where immersive environments could distract patients from their discomfort, and rehabilitation, where engaging virtual exercises could aid in physical recovery.
In recent years, integrating artificial intelligence and machine learning with VR has further expanded its capabilities. Personalized treatment plans, real-time feedback, and adaptive learning systems have enhanced the effectiveness of VR applications in healthcare. Today, VR is not just a novel technology but a critical tool in the medical arsenal, continually evolving to meet the dynamic needs of patients and healthcare providers.
VR's historical trajectory underscores its transformative potential as we stand on the cusp of a new medical era. From its humble beginnings to its current role in revolutionizing patient care, VR continues to break new ground, offering innovative solutions that promise to reshape the future of healthcare.
Want to implement effective VR solutions?
APPLICATIONS OF VIRTUAL REALITY
The integration of VR into patient care is a testament to the relentless pursuit of innovation in healthcare
From training medical professionals and managing pain to providing therapy and enhancing surgical precision, VR is redefining the possibilities of modern medicine. As technology continues to evolve, the potential for VR to further revolutionize patient care is boundless, promising a future where healthcare is more effective, immersive, and patient-centered.
VR in medical training
Virtual Reality (VR) has revolutionized training medical professionals, offering an immersive and interactive platform for honing skills without the risks associated with real-life procedures. In medical training, VR provides realistic simulations of surgical procedures, emergency scenarios, and routine medical practices, enabling trainees to practice and perfect their techniques in a controlled environment.
One notable example is the use of VR by surgical residents to practice complex operations. Institutions like Stanford University School of Medicine have integrated VR simulations into their curriculum, allowing trainees to perform virtual reality in surgical training that mimics real-life conditions. This hands-on experience is invaluable, enabling medical students and professionals to gain confidence and proficiency before entering an operating room.
A compelling case study is the use of VR by over 100 residency programs in the US, where a VR platform called ‘Touch Surgery’ is used to simulate various surgical procedures. This platform provides step-by-step guidance and real-time feedback, enhancing the learning experience and improving surgical skills. The success of such programs is reflected in improved surgical outcomes and reduced procedural errors, underscoring the effectiveness of VR in medical training.
VR for pain management
The application of VR in pain management is a groundbreaking development that leverages immersive environments to alleviate pain and enhance patient comfort. The mechanism behind this involves diverting the patient's attention away from their pain through engaging and interactive virtual experiences. By immersing patients in soothing or stimulating VR environments, their pain perception is significantly reduced.
Clinical trials have demonstrated the effectiveness of VR in pain management. For instance, a study conducted by Cedars-Sinai Medical Center found that patients using VR during medical procedures reported a 24% reduction in pain scores compared to those who did not use VR. Patient testimonials further highlight the impact of VR on pain relief. One patient suffering from chronic pain described how VR transported them to a serene beach, providing a respite from their discomfort and reducing their reliance on pain medication.
Clinical evidence supports these positive outcomes, showcasing VR as a powerful tool for managing pain without the side effects of traditional pharmacological treatments.
Virtual reality therapy
Virtual Reality Therapy (VRT) is making significant strides in mental health and rehabilitation, offering innovative solutions for conditions such as anxiety, post-traumatic stress disorder (PTSD), and phobias. VRT allows patients to confront and manage their fears in a controlled and safe virtual environment, facilitating exposure therapy that can be tailored to individual needs.
Success stories abound in the realm of VRT. For example, the use of VR for treating PTSD in military veterans has shown promising results. The Virtual Reality Medical Center in San Diego has developed a VR-based exposure therapy program that immerses veterans in simulations of combat scenarios, helping them process and overcome traumatic experiences. Statistics reveal that this approach has led to significant reductions in PTSD symptoms, with many participants reporting improved mental health and quality of life.
In rehabilitation, VR creates engaging and interactive exercises that motivate patients and enhance recovery outcomes. For instance, stroke patients can participate in VR-based exercises that simulate daily activities, promoting motor function recovery and improving their ability to perform real-life tasks.
VR in surgery
Virtual Reality is transforming the surgical landscape by enhancing pre-surgical planning and procedural precision. Surgeons can now use VR to visualize and rehearse complex operations, allowing for meticulous planning and identifying potential challenges before the actual surgery.
One prominent example is the Cleveland Clinic's use of VR for pre-surgical planning in intricate heart surgeries. Surgeons create 3D models of patients' hearts using VR, enabling them to explore different surgical approaches and select the most effective one. This pre-operative visualization enhances precision during surgery, reducing the likelihood of complications and improving patient outcomes.
Furthermore, VR simulations train surgeons in new techniques and procedures. For instance, using VR in laparoscopic surgery training has improved agility and reduced the learning curve for new surgeons. Enhanced surgical precision and outcomes are a testament to the transformative impact of VR in the operating room.
BENEFITS
VR is transforming the landscape of modern medicine with its multifaceted benefits
Virtual Reality (VR) revolutionizes the healthcare ecosystem by providing innovative solutions that enhance patient care, streamline medical processes, and foster continuous education. The immersive nature of VR allows for personalized treatment plans, leading to improved patient outcomes across various medical disciplines. By reducing costs associated with traditional training and treatment methods, VR is a cost-effective investment for healthcare providers. Additionally, the advanced training capabilities of VR offer medical professionals realistic, hands-on experiences, ensuring they are well-prepared to handle complex medical scenarios with precision and confidence.
Improved patient outcomes
Virtual Reality (VR) has ushered in a new era of patient care, marked by significantly improved outcomes across various medical disciplines. The immersive nature of VR allows for highly personalized and engaging treatment plans, which can be tailored to meet each patient's specific needs. For instance, VR distracts patients from their discomfort in pain management by immersing them in captivating virtual environments, resulting in reduced pain perception and a decreased need for pain medications. This approach alleviates suffering and mitigates the risks associated with long-term pharmacological treatments.
In surgical applications, VR enables meticulous pre-surgical planning and simulation, allowing surgeons to rehearse complex procedures in a virtual setting. This practice enhances precision, fewer surgical errors, and faster patient recovery times. Furthermore, VR-based rehabilitation programs offer interactive and motivating exercises, promoting better adherence to therapy and accelerated recovery. These benefits translate into improved patient satisfaction and overall better health outcomes, making VR an invaluable tool in modern medicine.
Cost-effectiveness
The integration of VR in healthcare also brings substantial cost-saving benefits. By reducing the need for physical resources and minimizing procedural errors, VR helps lower healthcare costs significantly. In medical training, VR simulators eliminate the need for expensive cadavers and traditional training materials, providing a cost-effective software solution that offers repeatable and customizable training scenarios. This reduction in training costs allows institutions to allocate resources more efficiently and focus on improving patient care.
Additionally, VR applications in pain management can decrease the reliance on costly pain medications and their associated side effects, leading to lower long-term healthcare expenses. By enhancing surgical precision, VR reduces the likelihood of complications and the need for additional corrective surgeries, further cutting down healthcare costs. These long-term savings quickly offset the initial investment in VR technology, making it a financially viable solution for healthcare providers.
Enhanced training and education
The educational potential of VR in healthcare is unparalleled. It offers a dynamic and interactive learning platform for medical professionals. VR simulations provide realistic, hands-on training experiences crucial for developing the skills and confidence needed in high-stakes medical environments. Medical students and trainees can practice complex procedures repeatedly in a safe, controlled setting, receiving real-time feedback that enhances their learning and competency.
One of VR's most significant advantages in medical training is the ability to simulate rare and complex cases that may not be frequently encountered in real-life clinical settings. This exposure ensures that medical professionals are well-prepared to handle various scenarios, improving their diagnostic and procedural skills. Institutions like the Mayo Clinic and Johns Hopkins University have successfully integrated VR into their training programs, resulting in more proficient and confident healthcare providers.
Moreover, VR offers continuous professional development opportunities for practicing clinicians. By engaging in VR-based training modules, surgeons can stay updated on the latest techniques and technologies, ensuring they maintain their expertise and deliver the highest standard of care. This continuous learning approach fosters a culture of excellence and innovation in healthcare.
Interested in introducing VR into your healthcare services?
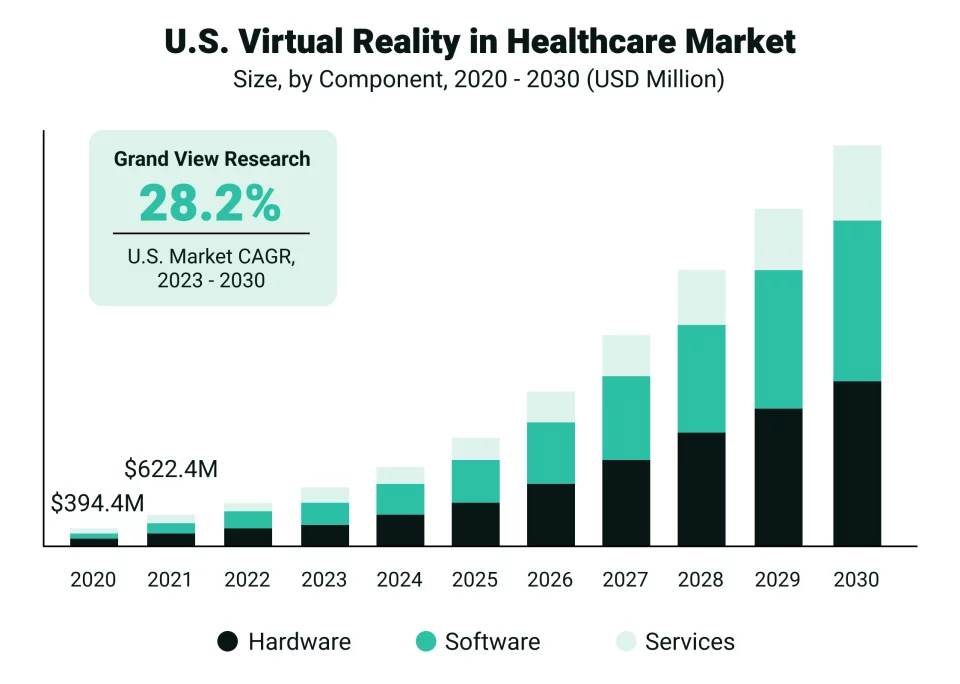
The growth of VR in the healthcare market is inevitable
CHALLENGES
VR presents significant hurdles for healthcare organizations that restrict its smooth implementation
While Virtual Reality (VR) is making remarkable strides in healthcare, it is not without its limitations and challenges. One of the primary obstacles is the high cost of VR technology. The initial investment in VR hardware and software can be substantial, posing a barrier for many healthcare institutions, particularly smaller practices with limited budgets. Additionally, the integration of VR into existing healthcare systems requires significant infrastructural changes and training for medical professionals, which can be both time-consuming and costly.
Another challenge is the need for robust clinical validation. Although numerous studies highlight VR's benefits in patient care, comprehensive, large-scale clinical trials are necessary to establish standardized protocols and best practices. The absence of standardized guidelines can lead to inconsistent application and varying outcomes, hindering the widespread adoption of VR in healthcare.
Technical limitations also present hurdles. VR systems require high-performance computing power and advanced graphics capabilities to deliver realistic and immersive experiences. Any lag or technical glitches can disrupt the user experience and diminish the therapeutic benefits. Moreover, issues related to user comfort, such as motion sickness and eye strain, need to be addressed to ensure patient compliance and satisfaction.
FUTURE PROSPECTS
VR’s future prospects look bright with its varied uses in patient treatment
Despite these challenges, the future prospects of VR in healthcare are up-and-coming. As technology advances, the cost of VR systems is expected to decrease, making them more accessible to a broader range of healthcare providers. Innovations in VR hardware, such as lighter and more comfortable headsets, will enhance user experience and reduce motion sickness and eye strain issues.
Future trends in VR healthcare will likely see greater integration with artificial intelligence (AI) and machine learning. These technologies can provide real-time data analysis and personalized feedback, further enhancing the effectiveness of VR applications. For instance, AI-driven VR systems can adapt to individual patient needs, offering tailored rehabilitation exercises or therapeutic environments that maximize treatment outcomes.
Telemedicine, another burgeoning field, stands to benefit significantly from VR advancements. Remote VR consultations can create immersive, face-to-face interactions between patients and healthcare providers, bridging geographical gaps and improving access to quality care. VR can also facilitate remote training and collaboration among medical professionals, fostering a global exchange of knowledge and expertise.
Moreover, VR's potential in surgical planning and training will continue to expand. Future developments might include more sophisticated simulations incorporating real-time patient data, allowing surgeons to practice personalized procedures with unprecedented accuracy. This will improve surgical outcomes and accelerate the learning curve for new and complex techniques.
As technological advancements drive down costs and enhance capabilities, VR is set to become an indispensable tool in modern medicine. Its potential to revolutionize patient care, medical training, and mental health treatment heralds a new era where immersive, innovative solutions are at the forefront of healthcare advancements.
VR can transform the way you deliver patient care
ASAHI'S ROLE
Take a look at Asahi Technologies’ role in advancing VR in healthcare
Asahi Technologies is at the forefront of leveraging cutting-edge VR technology to transform the healthcare landscape. With a deep understanding of both technological innovation and the specific needs of the medical field, we offer a comprehensive suite of VR solutions tailored to enhance patient care, medical training, and therapeutic interventions. Our services include the development of immersive VR training modules for medical professionals, interactive patient treatment plans, and customized rehabilitation programs. We ensure healthcare providers can access the most effective and user-friendly VR applications by integrating state-of-the-art VR hardware with advanced custom healthcare software development.
Why choose Asahi Technologies?
Choosing Asahi Technologies for VR solutions in healthcare offers several compelling advantages. First and foremost, our expertise in VR technology and the healthcare industry ensures we can deliver tailored solutions that meet the unique demands of medical professionals and patients. We strongly emphasize collaboration and client satisfaction and work closely with healthcare providers to understand their needs and challenges, developing customized VR applications that directly address these requirements.
We are dedicated to ensuring the accessibility and usability of our VR solutions. Our team provides comprehensive training and support to healthcare providers, ensuring that medical professionals can seamlessly integrate VR into their practice and maximize its benefits. We design user-friendly solutions, minimizing the learning curve and making it easy for both healthcare providers and patients to adopt and utilize the technology effectively.
CONCLUSION
VR has the power to improve healthcare delivery and improve patient outcomes
Virtual Reality (VR) revolutionizes patient care by offering innovative, immersive solutions that enhance medical training, improve patient outcomes, and provide effective pain management and mental health therapies. Despite challenges such as cost and technical limitations, the future of VR in healthcare is bright, with trends pointing towards increased integration and wider adoption. As we embrace these advancements, the potential for VR to transform healthcare practices becomes increasingly apparent, promising a future where patient care is more precise, personalized, and accessible. By harnessing the power of VR, we are not just improving healthcare; we are redefining it for the better.
Want user-friendly VR solutions to help patients get better?
People Also Ask (PAA) questions
- How is virtual reality used in healthcare?
Virtual reality (VR) is used in healthcare for medical training, surgical simulations, pain management, and mental health therapy. It creates immersive environments for realistic practice and therapeutic experiences. - What are the benefits of VR in patient care?
VR enhances patient outcomes by providing immersive, personalized treatment plans, reducing pain perception, and improving recovery times. It also offers cost-effective training and therapeutic solutions. - Can virtual reality help in pain management?
Yes, VR helps in pain management by distracting patients with immersive environments, reducing their perception of pain. Clinical trials have shown significant reductions in pain levels during VR sessions. - What is virtual reality therapy?
Virtual reality therapy (VRT) uses immersive VR environments to treat mental health conditions and aid in rehabilitation. It is effective for anxiety, PTSD, phobias, and physical therapy. - How does VR improve surgical outcomes?
VR improves surgical outcomes by allowing surgeons to rehearse complex procedures in a virtual setting. This practice enhances precision, reduces errors, and leads to faster patient recovery. - What are the challenges of using VR in healthcare?
Challenges include high costs, technical limitations, the need for extensive clinical validation, and ensuring user comfort. Integrating VR into existing healthcare systems also requires significant training. - How does VR training benefit medical professionals?
VR training provides realistic, hands-on practice in a safe environment, enhancing skills and confidence. It allows for repeated practice of complex procedures, improving overall competency and readiness. - What are some examples of VR applications in healthcare?
Examples include VR surgical simulations, pain management systems, mental health therapy, and rehabilitation programs. VR is also used in medical education to simulate rare and complex cases. - How does virtual reality help in mental health treatment?
VR helps in mental health treatment by providing controlled, immersive environments for exposure therapy. It is effective for treating anxiety, PTSD, and phobias, offering personalized therapeutic experiences. - Why is VR considered a breakthrough in patient care?
VR is considered a breakthrough because it offers innovative, immersive solutions that enhance treatment effectiveness, improve patient outcomes, and provide cost-effective training and therapeutic options.






